Meningioangiomatosis
This is a rare malformation of the central nervous system, so rare that not many cases of cystic Meningioangiomatosis (MA) have been reported. First described by Bassoe and Nuzum in 1915, Meningioangiomatosis was found incidentally in an autopsy of a 15-year old boy. It is characterized by a plaque-like or nodular mass overlapping leptomeninges in patients.
Though the pathogens are unknown, there are three possible theories – first, these lesions probably represent a hamartoma - a benign malformation made up of an abnormal mixture of cells and tissues. Second, they could result from direct invasion of the brain tissue by a leptomeningeal meningioma. Third, they represent a vascular malformation.
A rare disease characterized by the brain, benign lesion of the leptomeninges, MA usually involves the cerebral cortex. Seizures are often noticed in these patients. Though extremely rare multifocal cases have been reported both in adults and children, the lesion is normally found in one place. Biopsy is necessary for diagnosis and conventional treatment is to surgically remove the lesion.
Meningioangiomatosis may either be sporadic or associated with Neurofibromatosis type 2. In sporadic Meningioangiomatosis, seizures and headaches are present. Whereas, NF2 is asymptomatic and diagnosed only at autopsy. Meningioangiomatosis is benign and the seizures can be surgically corrected.
Analysis
When medical records of ten histopathologically confirmed MA patients were treated between 2010 and 2011, all the patients presented with symptomatic seizure attacks before surgery. MRI and CT were the radiological examinations done for pre-operative diagnosis of all cases. Accurate diagnosis of Meningioangiomatosis is important because it is a benign surgically correctable cause of seizures.
Results
All patients underwent craniotomy surgeries with total gross resections of MA lesions.
Post operative follow-ups range from 8 to 108 months. No radiological recurrence was found in any case. While eight patients achieved total symptomatic remission after surgeries, two were found to suffer from attacks infrequently under severe anti-epileptic drugs.
Although MA is rare and usually misdiagnosed, it is possible for correct preoperative diagnosis with differential diagnosis taking into consideration patient's ages, symptomatic seizure attacks, and radiological findings. MA is curable and the prognosis is excellent since patients become free of seizure after surgical treatments.
Deep Brain Stimulation
Deep brain stimulation is a specialized neurosurgical treatment option for patients suffering from a special group of neurological disorders called 'Movement Disorders'. Deep Brain Stimulation or DBS is an advanced procedure performed by neurosurgeons for treating patients who cannot achieve optimal results through conventional medical therapy alone.
Neurophysiology of Movement Disorders
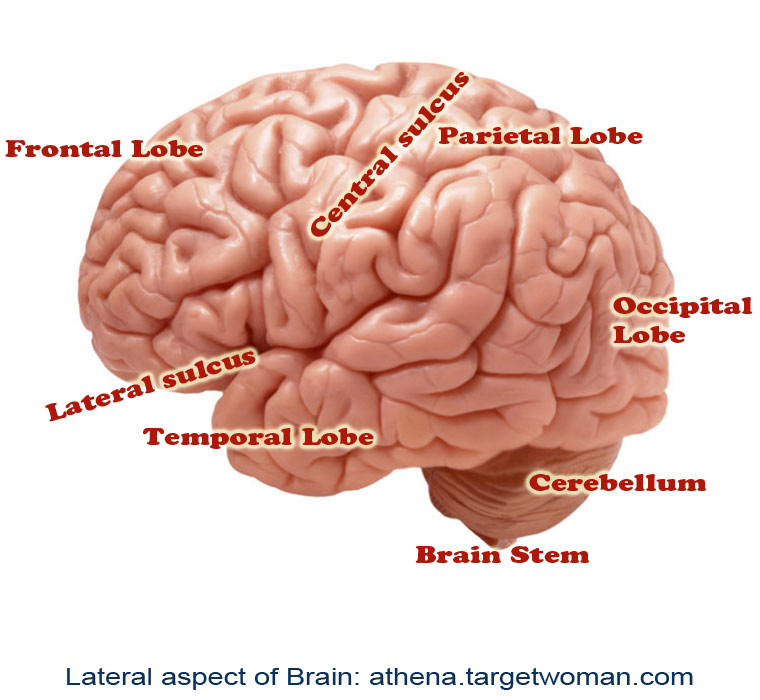
Movement disorders refer to conditions associated with changes in specific areas of the nervous system which results in abnormal involuntary movements, slow or reduced movements. The two main areas of the brain which are affected in movement disorders are the basal ganglia and the sub-thalamic nucleus. The disorders are classified into various groups such as hypokinetic disorders (e.g.: Parkinsons), hyperkinetic disorders (e.g.: Huntington's disease), and Non-motor disorders (e.g.: Tourette's Syndrome and Obsessive Compulsive Disorders). When these nuclei start having abnormal electrical activity (discharging too much or too little), the patient experiences specific symptoms related to movement.
Indications for Deep Brain Stimulation
Deep brain stimulation is used for patients who usually suffer from movement disorders such as Parkinsons, tremors, and dystonia. It is called Deep Brain Stimulation because surgically placed electrodes are used to stimulate specific areas (nuclei) deep inside the brain. The most common nuclei commonly stimulated are the Globus Pallidus and the sub-thalamic nuclei.
The idea behind DBS is that it functions somewhat like a 'pacemaker' in the brain, periodically sending electrical signals to the specific nuclei, thereby modulating the effect of these nuclei. Hence, DBS is also called as neuromodulation therapy'. In DBS, specific electrical signals are sent to the abnormally functioning nuclei to reduce or increase their activity.
Components
There are three components of the Deep Brain Stimulation system. They are:
The Stimulating Electrodes
The IPG – Internal Pulse Generator (the pacemaker)
The Extension - connecting leads between the Electrode and IPG.
The IPD contains a battery pack which has to be replaced every 4 years. The IPG is programmed by the neurologist based on the specific disease condition of the patient, and the placement of DBS requires regular follow-ups for programming the IPG based on the disease condition, if needed.
Procedure
Specialized Brain Mapping technology is used to locate the specific nuclei which are suspected to be abnormally functioning. These nuclei are the 'target area' for DBS. A specially designed stereotaxic frame is attached to the patient's head which provides a three-dimensional reference system for the patient's brain and enables the neurosurgeon to precisely locate the nuclei or track the electrode tip during placement.
The procedure normally takes up to three hours and is performed by a neurosurgeon specially trained in the procedure. The surgery is called awake craniotomy since the patient is awake during the entire duration of the procedure so that his neurological functions can be assessed in real-time to see the 'before and after' results due to the electrode placement. Following the placement of the electrodes, the IPGs are implanted either during the time of the surgery or later on. Each brain is unique, and hence the IPGs have to be specially programmed and the settings have to be specific for each patient. This is usually done about 2 weeks after the electrode placement.
Clinical Results
It is not exactly known how DBS functions, but there have been marked clinical improvements for patients with Parkinson's disease, tremors, and dystonia. Although a large percentage of patients report significant improvement after DBS surgery, there is no guarantee that DBS will help every patient with movement disorder.
Patients with Parkinson's report 60-80% improvement in tremor and slowness of movement. Patients on an average report 50% improvement in their walking and balance following DBS. Others with dyskinesia (involuntary movements) report more than 80% improvement following DBS.
Complications
Although DBS on the whole has proven safe and effective, there is a possible 2-3% risk of intra-cranial hemorrhage and meningitis due to leakage of cerebro-spinal fluid. There is a 15% chance of developing infection due to the placement of the electrodes. There is a possibility that seizures may occur, if the tip of the electrode migrates, thereby stimulating other areas of the brain. However such findings have not been reported until now.
Future of DBS
Besides movement disorders, DBS has been used to chronic pain, and currently possibilities of using DBS for other cognitive disorders such as severe depression, obsessive compulsive disorder, eating behavioral disorders and drug addiction, are underway.
Brain Cancer
Malignant tumors in the brain are the consequence of abnormal growth of cells in the brain. Brain cancers can be primary, arising from primary brain cells, or from other brain components. Metastatic brain cancer starts elsewhere in the body and spreads to the brain. About 25% of tumors elsewhere in the body metastasize to the brain. The most common cancers that metastize to the brain are lung cancer, breast cancer, colon cancer and melanoma. The majority of brain metastases are located in the cerebral hemispheres and then in the cerebellum. Very few occur in the brain stem.
Causes/ risk factors for brain cancer
- Any radiation to the head
- Hereditary
- HIV infection
- Smoking
- Toxins found in the environment such as chemicals in oil refinery, rubber industry chemicals etc)
Symptoms of Brain Cancer
- Severe headache in the morning.
- Nausea and vomiting, especially early in the mornings.
- Some changes/problems while talking, listening or seeing.
- Problems while walking.
- Memory problems or lack of alertness.
- Twitching of muscles or seizures.
- Numbness in the arms or legs.
- General weakness
- Clumsiness
- Gradual changes in intellectual and emotional capacity.
These symptoms may be very gradual and therefore overlooked by the patient. Occasionally however, these symptoms may appear more rapidly.
Who is at risk for brain cancer ?
Persons with the following conditions are at more risk for developing cancer of the brain.
- Frequent exposure to radiation
- Age
- Exposure to pesticides, herbicides and fertilizer
- Workers occupied in petroleum, plastic, rubber and textile industries.
- Exposure to electromagnetic fields
- Genetic disorders
Diagnosis of Brain Cancer
MRI has higher sensitivity for detecting the presence and characteristics of a tumor. In case, the CT or MRI indicates the presence of a brain tumor, the patient will be referred to a neurosurgeon or to a neuro oncologist. The next step in diagnosis is to confirm cancer in the brain. A biopsy is taken to identify the type of tumor and the grade of the tumor. This is done by a surgical procedure called craniotomy. The skull is opened with the intention of removing the whole tumor if possible. A biopsy is taken from the tumor. In some cases, if the exact location of the tumor is detected, by using a CT or MRI scan, a biopsy is taken without opening the skull. This technique is stereotaxis, where a needle is used to collect the biopsy. A pathologist examines the biopsy under a microscope and diagnoses the disease.
Brain cancer treatment
Treatment for brain cancer is based on the patient's age, and general health status, size, location and type and grade of the tumor. In most cases of brain cancer, surgery, radiation and chemotherapy are the preferred treatment. As treatment protocols of brain cancer are highly complex, most treatment plans will involve several consultations and sittings with the neurosurgeon, oncologist, radiation oncologist and healthcare provider.
Most people with brain cancer undergo surgery to assign and grade the tumor and then remove the tumor or take a sample to identify the type and grade. In some cases, a benign tumor can be cured by surgical intervention and removal of tumor.
Stereotactic radio surgery, a knife less technique that can destroy a brain tumor without opening the skull can be adopted. With a CT or MRI, the exact location is pinpointed and with high energy radiation beams the tumor from different angles is destroyed. Knife less procedure has fewer complications and the recovery time is shorter. The disadvantage is the lack of tissue available to send to a pathologist for diagnosis of brain swelling.
Radiation can be administered externally or internally. External radiation travels through skin and the skull, healthy brain tissue and other tissues to get to the tumor. Internal radiation uses a tiny radioactive capsule placed inside the tumor itself. The radiation emitted from the capsule destroys the tumor.
Chemotherapy drugs may be administered by mouth or through an IV line. Chemotherapy is usually administered in cycles, each cycle consisting of a short period of intensive treatment followed by a period of rest and recovery. The side effects of chemotherapy include nausea, vomiting, mouth sores, loss of appetite, loss of hair among others. New therapies with the use of nanotechnology for cancer are being developed and are promising. Regular follow up is essential after treatment of brain cancer. Such checkups would include physical and neurologic exams, and occasional CT and/or MRI.
Tags: #Meningioangiomatosis #Deep Brain Stimulation #Brain Cancer
At TargetWoman, every page you read is crafted by a team of highly qualified experts — not generated by artificial intelligence. We believe in thoughtful, human-written content backed by research, insight, and empathy. Our use of AI is limited to semantic understanding, helping us better connect ideas, organize knowledge, and enhance user experience — never to replace the human voice that defines our work. Our Natural Language Navigational engine knows that words form only the outer superficial layer. The real meaning of the words are deduced from the collection of words, their proximity to each other and the context.
Diseases, Symptoms, Tests and Treatment arranged in alphabetical order:

A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
Bibliography / Reference
Collection of Pages - Last revised Date: February 23, 2026



