Deep Brain Stimulation
Deep brain stimulation is a specialized neurosurgical treatment option for patients suffering from a special group of neurological disorders called 'Movement Disorders'. Deep Brain Stimulation or DBS is an advanced procedure performed by neurosurgeons for treating patients who cannot achieve optimal results through conventional medical therapy alone.
Neurophysiology of Movement Disorders
Movement disorders refer to conditions associated with changes in specific areas of the nervous system which results in abnormal involuntary movements, slow or reduced movements. The two main areas of the brain which are affected in movement disorders are the basal ganglia and the sub-thalamic nucleus. The disorders are classified into various groups such as hypokinetic disorders (e.g.: Parkinsons), hyperkinetic disorders (e.g.: Huntington's disease), and Non-motor disorders (e.g.: Tourette's Syndrome and Obsessive Compulsive Disorders). When these nuclei start having abnormal electrical activity (discharging too much or too little), the patient experiences specific symptoms related to movement.
Indications for Deep Brain Stimulation
Deep brain stimulation is used for patients who usually suffer from movement disorders such as Parkinsons, tremors, and dystonia. It is called Deep Brain Stimulation because surgically placed electrodes are used to stimulate specific areas (nuclei) deep inside the brain. The most common nuclei commonly stimulated are the Globus Pallidus and the sub-thalamic nuclei.
The idea behind DBS is that it functions somewhat like a 'pacemaker' in the brain, periodically sending electrical signals to the specific nuclei, thereby modulating the effect of these nuclei. Hence, DBS is also called as neuromodulation therapy'. In DBS, specific electrical signals are sent to the abnormally functioning nuclei to reduce or increase their activity.
Components
There are three components of the Deep Brain Stimulation system. They are:
The Stimulating Electrodes
The IPG – Internal Pulse Generator (the pacemaker)
The Extension - connecting leads between the Electrode and IPG.
The IPD contains a battery pack which has to be replaced every 4 years. The IPG is programmed by the neurologist based on the specific disease condition of the patient, and the placement of DBS requires regular follow-ups for programming the IPG based on the disease condition, if needed.
Procedure
Specialized Brain Mapping technology is used to locate the specific nuclei which are suspected to be abnormally functioning. These nuclei are the 'target area' for DBS. A specially designed stereotaxic frame is attached to the patient's head which provides a three-dimensional reference system for the patient's brain and enables the neurosurgeon to precisely locate the nuclei or track the electrode tip during placement.
The procedure normally takes up to three hours and is performed by a neurosurgeon specially trained in the procedure. The surgery is called awake craniotomy since the patient is awake during the entire duration of the procedure so that his neurological functions can be assessed in real-time to see the 'before and after' results due to the electrode placement. Following the placement of the electrodes, the IPGs are implanted either during the time of the surgery or later on. Each brain is unique, and hence the IPGs have to be specially programmed and the settings have to be specific for each patient. This is usually done about 2 weeks after the electrode placement.
Clinical Results
It is not exactly known how DBS functions, but there have been marked clinical improvements for patients with Parkinson's disease, tremors, and dystonia. Although a large percentage of patients report significant improvement after DBS surgery, there is no guarantee that DBS will help every patient with movement disorder.
Patients with Parkinson's report 60-80% improvement in tremor and slowness of movement. Patients on an average report 50% improvement in their walking and balance following DBS. Others with dyskinesia (involuntary movements) report more than 80% improvement following DBS.
Complications
Although DBS on the whole has proven safe and effective, there is a possible 2-3% risk of intra-cranial hemorrhage and meningitis due to leakage of cerebro-spinal fluid. There is a 15% chance of developing infection due to the placement of the electrodes. There is a possibility that seizures may occur, if the tip of the electrode migrates, thereby stimulating other areas of the brain. However such findings have not been reported until now.
Future of DBS
Besides movement disorders, DBS has been used to chronic pain, and currently possibilities of using DBS for other cognitive disorders such as severe depression, obsessive compulsive disorder, eating behavioral disorders and drug addiction, are underway.
Prion Disease
Prion diseases are Transmissible Spongiform Encephalopathies or TSE that affect humans and animals. In humans, they cause neurological disorders that are progressively degenerative. A prion is an abnormal pathogen that affects proteins found in the brain causing them to fold and clump unnaturally. This then leads to brain damage that is progressive. Prion diseases may occur spontaneously, may be inherited or may be acquired from contaminated material.
The most common form of prion disease is Creutzfeldt Jakob Disease or CJD. A variant of CJD is the 'mad cow disease'. The infection passes on to humans through contaminated meat. The most common pathologic feature of CJD is the formation of vacuoles (fluid filled spaces) in the brain giving rise to sponge-like appearance. CJD is one of several spongiform encephalopathies. Others include Kuru and Gerstmann Straussler Scheinker Syndrome.
Typical symptoms of prion disease include muscle stiffness, dementia, hallucinations, ataxia and fatigue. There is a change in the personality and behavior of the person. Diagnostic tests such as brain MRI, Spinal tap, EEG and blood tests are done to understand the condition. Brain tissue biopsy helps to confirm the disease. With rapid progression of the disease, the patient needs help in taking care of himself and might need to be moved to assisted care.
Kuru is another degenerative human spongiform encephalopathy disease that afflicted the Fore people from Papua, New Guinea due to ritual cannibalism.
GSS or Gerstmann Straussler Scheinker Syndrome is a rare neurological disorder due to brain degeneration. It is mostly inherited and sets in middle age. Initially the patient suffers cerebellar ataxia (lack of muscular coordination) and gradually deteriorates to dementia. There might be Nystagmus (rapid involuntary eye movements) and visual problems. There is a possibility of developing Parkinsons disease too. With rapid progression of the disease, the patient needs help in taking care of himself and might need to be moved to assisted care.
FFI or Fatal Familial Insomnia is a type of prion disease where the patient has difficulty in walking and falling asleep. There might be weight loss and excessive tears in the eye. It rapidly deteriorates to loss of consciousness and death. Initially the patient suffers insomnia that later worsens to include panic attacks, phobia and hallucinations. There might be weight loss and incontinence. After this, the patient might suffer dementia and sudden death.
Pick's Complex
This is a less common form of dementia, more prominent in those under the age 65. Frequently misdiagnosed as Alzheimer's disease, Pick's patients initially exhibit marked personality and behavioral changes. And gradually the ability to speak coherently declines.
Although there is no cure for Pick's complex presently, it can however be managed well and the quality of life improved. According to Arnold Pick, who first described the disease in 1892, Pick's disease causes an irreversible decline in a person's functioning for several years. Pick's affects adults between the ages of 40 and 60 and is more common in women than men.
Causes
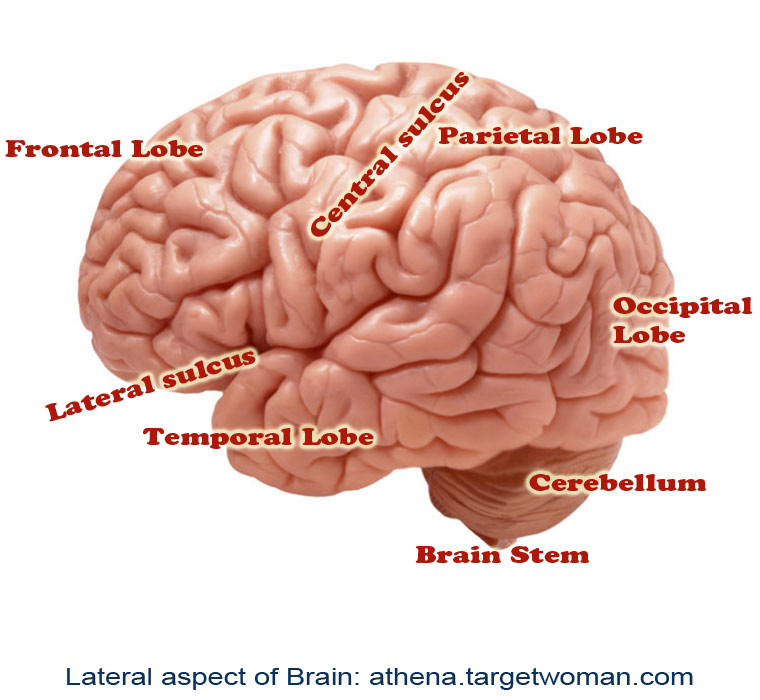
The frontal and temporal lobes of the brain control a person's speech and personality. Excess protein build-up in these parts causes slow atrophy in these regions. The cause for this build-up of protein is unknown. Other than causing speech and behavioral changes, Pick's disease can also cause memory loss quite like those with Alzheimer's as well as socially inappropriate behavior, poor decision making, progressing to severe impairment in intellect, speech and memory. Some opine that Pick's disease may have a genetic or heredity component although not all family members are affected.
Symptoms of Pick's disease
The first sign of Pick's complex is personality changes and decline of basic functioning. Pick's can occur in an age earlier than Alzheimer's and memory loss need not be a predominant early sign of Pick's disease. Although there could be reports of Pick's occurring as young as 20 years of age, the progression is slower in Pick's disease. However, there are cases where symptoms could worsen over time and brain cells degenerate. More severe symptoms appear at later stages of Pick's. Some noticeable behavioral symptoms of Pick's disease are poor judgment, extreme restlessness especially in the early stages, overeating or drinking, lack of personal hygiene, sexual exhibitionism, decreased interest in daily activities and obsessive behavior.
Mood swings, lack of empathy, apathy, rudeness, impatience and aggression, easy distraction and being unaware of strange behavior and memory loss are some of the prominent emotional symptoms of Pick's disease. Loss of vocabulary, difficulty in speaking and understanding, uncoordinated speech and decrease in the ability to speak and write are some serious signs of Pick's.
Diagnosis of Pick's Complex
Other than careful symptomatic evaluation, brain scans and EEG, three of the following five characteristics are found to be present in the early stages. They include:
-
Onset before age 65
Personality changes
Lack of normal behavior / Loss of control
Lack of inhibition
Roaming behavior
When compared to Alzheimer's, memory loss and mental impairment occur later in Pick's.
Diet and activity
There should be a restriction on foods with high sugar content. There could be carbohydrate cravings in some. While in Alzheimer's and Parkinsons, a diet relatively high in fat and protein and low in carbohydrates is necessary, it is unclear if the same is recommended for Pick's complex. It is better to get a doctor's opinion on an appropriate heart-healthy diet. A regimen of therapeutic exercises such as brisk walking can help to regulate the patient's mood and benefit on cognitive function.
Treatment
Pick's disease, like any other dementia progresses rapidly and life gets shortened about six to eight years, although some do live for as long as twenty years. As currently there is no cure for Pick's like Alzheimer's, the aim is to maximize quality of life by way of medications to manage particular symptoms, regular supervision, and assistance.
Emotional and substantive support is an important aspect of the treatment. The family of the affected may help with the following control symptoms:
- Eyeglasses and hearing aids to bolster the failing senses.
- Positive behavior when symptoms set in by creating a calm and soothing atmosphere so that the patient feels safe and less anxious.
- Speech therapy or any other physical therapy that can improve communication and movement.
- Selective antidepressants that can provide some relief from apathy and depression and help reduce food cravings, impulse control and compulsive activity.
- Treatment for other disorders such as anemia, thyroid disorders and kidney or liver diseases.
- Stopping medications like paracetamol, NSAIDS, anti-cholergenics or changing them under medical guidance.
Tips for coping with Pick's complex
Being diagnosed with Pick's complex can be overwhelming especially when it involves any form of dementia. It is good to learn more about Pick's disease and frontotemporal dementia. In this way, more control can be exhibited and they will be better prepared to manage symptoms.
- Music therapy, meditation, deep breathing exercises can help control stress and anxiety.
- Pet therapy and visits from specially trained animals can help relieve stress and improve mood.
- Treating depression can make it easier to handle other challenges of the disease.
- Reaching out to family and friends for emotional support can help avoid isolation. A support group of similar patients can help overcome feelings of depression and isolation and provide a wealth of coping tips. Staying socially active will lighten the load and increase patient comfort.
- Playing cards and word games such as scrabble, crossword and Sudoku puzzles can exercise the brain and help slow cognitive decline.
- It would be wise for a Pick's patient to avoid medical, financial and legal confusion and instead create a design plan and discuss and document end-of-life preferences with doctors and family members.
Tags: #Deep Brain Stimulation #Prion Disease #Pick's Complex
At TargetWoman, every page you read is crafted by a team of highly qualified experts — not generated by artificial intelligence. We believe in thoughtful, human-written content backed by research, insight, and empathy. Our use of AI is limited to semantic understanding, helping us better connect ideas, organize knowledge, and enhance user experience — never to replace the human voice that defines our work. Our Natural Language Navigational engine knows that words form only the outer superficial layer. The real meaning of the words are deduced from the collection of words, their proximity to each other and the context.
Diseases, Symptoms, Tests and Treatment arranged in alphabetical order:

A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
Bibliography / Reference
Collection of Pages - Last revised Date: February 23, 2026



