Spherocytosis
Hereditary Spherocytosis is a genetic disorder characterized by red blood cells that are fragile and spherical in shape instead of the normal flat disk shape. The abnormal shape makes it difficult for red blood cells to pass through the spleen. The spleen's function is to purify the blood and safeguard the immune function by fighting against the potentially dangerous bacteria, viruses or other microorganisms in the blood. In case of Spherocytosis, the membrane of the red blood cells is defective lending it a spherical shape. When these defective blood cells pass through the spleen, they break and destroy causing premature death of the red blood cells. The shortage of blood cells gives rise to severe anemia. It is an inherited type of Hemolytic Anemia. A parent with the disease has a 50% chance of having a child with the disease. Spherocytosis is most common in people of northern European descent.
Symptoms
The symptoms can vary from mild to severe. In severe cases, the disorder may be found in early childhood. In mild cases it may go unnoticed until adulthood. Patients with Spherocytosis exhibit all the symptoms associated with anemia such as fatigue, irritability, shortness of breath and muscle weakness. They also appear pale and weak. In addition to these symptoms, Spherocytosis also causes enlarged spleen and jaundice with yellow skin and eyes. Jaundice occurs due to the elevated levels of serum bilirubin as the red blood cells are destroyed within the body. Excess bilirubin, sometimes, also results in in the gallbladder. These stones may cause pain, infection or may block the tubes that lead out of the gallbladder.
Diagnosis
Family history is checked for hereditary factor and the abdomen has to be checked for enlarged spleen. Following blood tests may be performed to support the clinical examination:
- CBC or complete blood count test to check for anemia.
- The Reticulocyte Count Test is performed to measure the new and immature red blood cells produced in the bone marrow. The reticulocyte count is usually higher in cases of Spherocytosis.
- Osmotic Fragility Test is performed to measure the fragility of the red blood cells. This involves taking a blood sample and suspending in a salt solution and then measuring the destruction and fragility of the cells.
- Coombs Test to measure the antibodies in the blood.
- Blood test to check for bilirubin levels.
Treatment
Splenectomy is the most definitive treatment for hereditary Spherocytosis. By removing the spleen, red blood cells are prevented from damage and are allowed to stay alive for a longer duration. However, removing a spleen makes the patient susceptible to infections for a lifetime. Hence patients need to take penicillin (or another antibiotic) for the rest of their lives. Immunization against pneumococcal and meningococcal infections is also prescribed. In case of severe anemia, blood transfusion is advised.
Fifth Disease
Fifth disease, also known as Erythema Infectiosum or Slapped Cheek Syndrome, is a viral infection caused by parvovirus B19 that leads to a rash on the cheeks, arms, and legs. It is known as fifth disease as Parvovirus infection is one of the five common illnesses that develop with red rash during childhood. It is most common in children between the age group of 5 and 15 and usually occurs in winter and spring. Fifth disease usually is a mild illness. It is contagious and spreads through direct contact with fluids or mucus from the nose or mouth of an infected person. Though rare, adults can also become infected with virus and develop fifth disease. However, the symptoms and the severity of the disease vary between children and adults.
Symptoms
The symptoms of fifth disease almost resemble flu with mild fever, headache, cough runny nose and muscle ache. Stomach related symptoms like nausea, vomiting and diarrhea may also develop in due course. These symptoms subside after 3 or 4 days and only then the red rash will start to surface, initially on the cheek and later spreading to arms, chest and even legs. The rash has a lace like pattern at the time of fading. At this stage, the disease is no longer contagious and the child can be allowed to attend school or day care. In adults, fifth disease also gives rise to joint pains, but this is very uncommon in children. The incubation period for fifth disease ranges from 4 to 28 days and the rash usually lasts for 1 to 3 weeks. Normally fifth disease is diagnosed after noticing the rash on the cheek.
Treatment
Fifth disease is rarely threatening and clears off on its own without any aggressive treatment. Doctors generally prescribe acetaminophen or ibuprofen to treat fever and other flu like symptoms. Adequate rest, plenty of fluids and avoiding exposure to sun and heat helps immensely in relieving the symptoms.
Complications
Fifth disease does not cause any complications in normal cases. However patients with certain underlying conditions such as autoimmune disorders, sickle-cell anemia, Aplastic anemia, Spherocytosis and low count of red blood cells need to be highly watchful of the disease as it can cause serious complications for them. They should seek immediate medical attention in case of suspicion to avoid further damage.
Fifth disease can also be dangerous to pregnant woman. In rare cases, the disease can spread from a pregnant woman to her unborn child. In such a condition, the baby will develop severe anemia with low red blood count leading to heart failure. Hence it is very important for pregnant women to avoid exposure to the disease and maintain hygiene throughout the term.
Prevention
There is no vaccine to prevent the infection and also no medication is available to treat it. It is best to prevent the disease by following certain steps like:
- Frequent washing of hands with medicated soap.
- Disposing used tissues or hand towels carefully.
- Covering your mouth when sneezing, coughing, etc.
- Avoiding contact with those who have Fifth disease.
RDW blood test
Red blood cell (RBC) indices are calculations derived from the complete blood count that helps in the process of diagnosis and classification of Anemia. A RBC indices blood test requires 3 to 5 ml of blood collected from a vein puncture.
RDW (Red cell Distribution Width) blood test that calculates any variation in size of RBC. Normally Red Blood Cells are of a standard size. Since RBCs tend to get smaller and rounder as they age, it is not possible for all cells to be exactly the same size. RDW test determines the changes in the volume of the cells in the red cell population. The variations pertaining to the size of the red blood cells is called Anisocytosis and the shape is called Poikilocytosis.
The incidence of these conditions and the detection of abnormal or varied red blood size are determined by diagnostic blood smear analysis and also through automated analyzers.
The following are the normal results for red blood cell indices ( a measurement of the variation in size of red blood cells):
- Mean Corpuscular Volume (measure of the average volume of a RBC) : MCV 82-98 femtoliters (fl)
- Mean Corpuscular Hemoglobin Concentration (measurement of the average concentration of hemoglobin in a RBC) : MCHC 33-37 g/dl
- Mean Corpuscular Hemoglobin (Measurement of the average weight of hemoglobin in a RBC): MCH 26-34 picograms (pg)
- RDW 11.5-14.5%
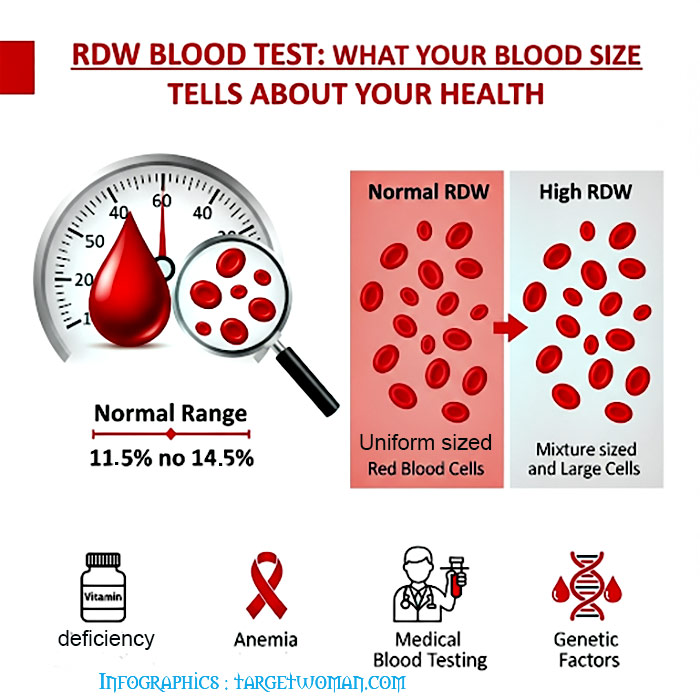
Normochromic: Indicates a normal concentration of hemoglobin. The RDW increases in anemia caused by deficiencies of Vitamin B12, iron or folic acid. Abnormal hemoglobin, as in sickle cell anemia, can result in changes in the shape of red blood cells. In addition it may also cause them to hemolyze. The abnormal shape and the cell fragments as a result of hemolysis would tend to increase the RDW. Severe blood loss may also induce immature cells into the blood that can increase the RDW.
Possible causes of abnormal MCV: MCV (Mean Corpuscular Volume) is an index of the size of the RBC. When the MCV is below normal, the RBC will be smaller than the normal size - which is known as microcytic. On the other hand, if the MCV is higher than normal, the RBC will also be larger than normal which is called as macrocytic while the normal RBC size is termed as normocytic.
High MCV: Macrocytic anemia owing to vitamin B12 and folic acid deficiency
Low MCV: Microcytic anemia, Thalassemia, poor iron content in diet and chronic illness
Normal MCV: Normocytic anemia owing to liver,kidney diseases, bone marrow disorders, hemolysis (distruction of red blood cells) or excessive bleeding
A low MCH (Mean Corpuscular Hemoglobin) is an indication that RBCs have too little hemoglobin. When viewed under the microscope, the RBCs appear pale and hence called as hypochromic. The MCHC (Mean Corpuscular Hemoglobin Concentration) is the ratio of RBC's hemoglobin mass to the cell volume. MCHC is elevated in hereditary Spherocytosis - as a result of the structural protein defect in the RBC.
Calculating Red Blood Cell Distribution: The determination of red cell distribution width is mathematically expressed as Red cell distribution width = (Standard deviation ÷ Mean cell volume) X 100.
Conditions such as pernicious anemia cause changes in RBC size. Often there is variation in shape too. This can be detected by changes in RDW. Normal RDW range is 11 - 15%. Higher RDW is indicative of disorders such as anemia. RDW blood test is often conducted along with MCV blood test to check the exact cause.
Tags: #Spherocytosis #Fifth Disease #RDW blood test
At TargetWoman, every page you read is crafted by a team of highly qualified experts — not generated by artificial intelligence. We believe in thoughtful, human-written content backed by research, insight, and empathy. Our use of AI is limited to semantic understanding, helping us better connect ideas, organize knowledge, and enhance user experience — never to replace the human voice that defines our work. Our Natural Language Navigational engine knows that words form only the outer superficial layer. The real meaning of the words are deduced from the collection of words, their proximity to each other and the context.
Diseases, Symptoms, Tests and Treatment arranged in alphabetical order:

A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
Bibliography / Reference
Collection of Pages - Last revised Date: February 23, 2026



