Deep Brain Stimulation
Deep brain stimulation is a specialized neurosurgical treatment option for patients suffering from a special group of neurological disorders called 'Movement Disorders'. Deep Brain Stimulation or DBS is an advanced procedure performed by neurosurgeons for treating patients who cannot achieve optimal results through conventional medical therapy alone.
Neurophysiology of Movement Disorders
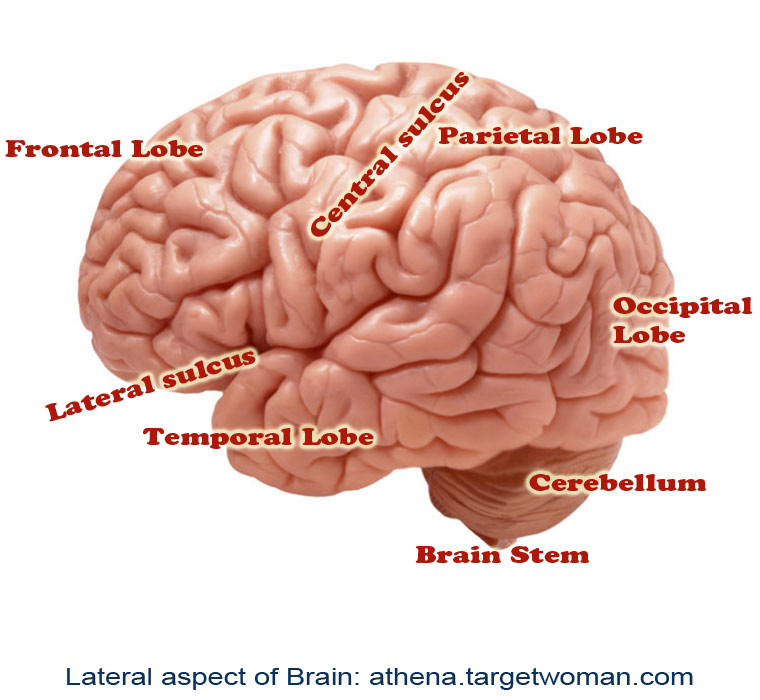
Movement disorders refer to conditions associated with changes in specific areas of the nervous system which results in abnormal involuntary movements, slow or reduced movements. The two main areas of the brain which are affected in movement disorders are the basal ganglia and the sub-thalamic nucleus. The disorders are classified into various groups such as hypokinetic disorders (e.g.: Parkinsons), hyperkinetic disorders (e.g.: Huntington's disease), and Non-motor disorders (e.g.: Tourette's Syndrome and Obsessive Compulsive Disorders). When these nuclei start having abnormal electrical activity (discharging too much or too little), the patient experiences specific symptoms related to movement.
Indications for Deep Brain Stimulation
Deep brain stimulation is used for patients who usually suffer from movement disorders such as Parkinsons, tremors, and dystonia. It is called Deep Brain Stimulation because surgically placed electrodes are used to stimulate specific areas (nuclei) deep inside the brain. The most common nuclei commonly stimulated are the Globus Pallidus and the sub-thalamic nuclei.
The idea behind DBS is that it functions somewhat like a 'pacemaker' in the brain, periodically sending electrical signals to the specific nuclei, thereby modulating the effect of these nuclei. Hence, DBS is also called as neuromodulation therapy'. In DBS, specific electrical signals are sent to the abnormally functioning nuclei to reduce or increase their activity.
Components
There are three components of the Deep Brain Stimulation system. They are:
The Stimulating Electrodes
The IPG – Internal Pulse Generator (the pacemaker)
The Extension - connecting leads between the Electrode and IPG.
The IPD contains a battery pack which has to be replaced every 4 years. The IPG is programmed by the neurologist based on the specific disease condition of the patient, and the placement of DBS requires regular follow-ups for programming the IPG based on the disease condition, if needed.
Procedure
Specialized Brain Mapping technology is used to locate the specific nuclei which are suspected to be abnormally functioning. These nuclei are the 'target area' for DBS. A specially designed stereotaxic frame is attached to the patient's head which provides a three-dimensional reference system for the patient's brain and enables the neurosurgeon to precisely locate the nuclei or track the electrode tip during placement.
The procedure normally takes up to three hours and is performed by a neurosurgeon specially trained in the procedure. The surgery is called awake craniotomy since the patient is awake during the entire duration of the procedure so that his neurological functions can be assessed in real-time to see the 'before and after' results due to the electrode placement. Following the placement of the electrodes, the IPGs are implanted either during the time of the surgery or later on. Each brain is unique, and hence the IPGs have to be specially programmed and the settings have to be specific for each patient. This is usually done about 2 weeks after the electrode placement.
Clinical Results
It is not exactly known how DBS functions, but there have been marked clinical improvements for patients with Parkinson's disease, tremors, and dystonia. Although a large percentage of patients report significant improvement after DBS surgery, there is no guarantee that DBS will help every patient with movement disorder.
Patients with Parkinson's report 60-80% improvement in tremor and slowness of movement. Patients on an average report 50% improvement in their walking and balance following DBS. Others with dyskinesia (involuntary movements) report more than 80% improvement following DBS.
Complications
Although DBS on the whole has proven safe and effective, there is a possible 2-3% risk of intra-cranial hemorrhage and meningitis due to leakage of cerebro-spinal fluid. There is a 15% chance of developing infection due to the placement of the electrodes. There is a possibility that seizures may occur, if the tip of the electrode migrates, thereby stimulating other areas of the brain. However such findings have not been reported until now.
Future of DBS
Besides movement disorders, DBS has been used to chronic pain, and currently possibilities of using DBS for other cognitive disorders such as severe depression, obsessive compulsive disorder, eating behavioral disorders and drug addiction, are underway.
Niemann pick
Niemann pick is a type of lysosomal storage disease and is an inherited condition that involves the metabolism of lipids. This leads to a breakdown in the of use and transport of fats and cholesterol in the body. The disease affects the body's ability to mobilize fat within cells. When this fat (cholesterol and lipids) accumulates in large amounts, it causes dysfunction of the cell and untimely death of a person. Harmful levels of lipids accumulate in the spleen, lungs, liver, bone marrow and brain. Niemann pick disease is more common in children. The disease is classified into three major types namely Niemann pick A, B and C. Niemann pick Type A and Type B are caused by the deficiency in an enzyme called acid sphingomyelinase. This enzyme is found within the lysosome cells and is an essential component in metabolizing a lipid called sphingomyelin.
Symptoms are related to the type of disease.
Type A: occurs in children. Children may not survive as the condition affects the nervous system. Symptoms include:
- Enlarged spleen and liver
- Progressive deterioration of the nervous system
- Stunted growth
- No weight gain.
Type B: occurs in childhood, known as the non-neurological type as the nervous system is not affected. Children survive into adulthood.
- Growth retardation
- Splenomegaly
- High cholesterol and lipid levels in the blood
- Low platelet levels
- Lung infection
- Problems in the functioning of the lungs.
Type C: can occur in children or in adults
- Severe liver disease
- Breathing difficulties
- Seizures
- Poor muscle tone
- Developmental delay
- Eye problem
- Problems in feeding
- Lack of coordination.
Other general symptoms include:
- Seizures
- Cataplexy (sudden loss of muscle tone)
- Dystonia (excessive muscle contraction)
- Accumulation of sphingomyelin in the central nervous system shows symptoms and signs like slurred speech (dysarthria) and abnormal swallowing (dysphagia)
- Recurrent pneumonia
- Difficulty in swallowing and eating
- Sleep disturbances
- Sleep inversion (sleepiness during the day and wakefulness during the night)
- Bones are affected.
Diagnosis depends on the type of Niemann pick disease
For Type A or B: Blood sample or bone marrow sample is used to measure the level of acid sphingomyelinase in the blood.
For Type C: A small sample is skin is taken to test how the cells move and store cholesterol.
Other tests may include brain MRI, genetic testing and eye test to confirm if there is difficulty in normal eye movement
Hallervorden spatz disease
Hallervorden Spatz disease or HSD is a rare neurological movement disorder that is passed down through families. It is characterized by progressive degeneration of the nervous system. According to the National Institute of Health, Hallervorden Spatz disease or its subtype affects less than 200,000 people in the US population.
Hallervorden Spatz disease was first described in 1922 as a form of brain degeneration characterized by iron deposition in the brain. The most recently used term for HSD is 'panthothenate kinase – associated neuro degeneration' as HSD specifically causes neuro degeneration and excessive iron accumulation. Onset of the disease is commonly in late childhood or early adolescence but there are cases with adult onset as well. The disease can be familial or sporadic. When familial it is inherited recessively.
Symptoms of Hallervorden spatz disease
- Motor disorder of extra pyramidal type and gait difficulty.
- Rigidity of extremities, slowness of movement.
- Predominant tremor – continuous shaking especially in the hands.
- Dystonia or involuntary muscle contractions – tight, weak and spastic muscles.
- Movement defects with uncontrollable twisting and squirming.
- Spasticity and dysarthria (speech disturbance caused by lack of control over muscles involved in speech) , brisk reflexes and extensor plantar responses.
- Significant disturbance in speech at an early age.
- Dementia is present in most individuals with HSD.
- Visual impairment from optic atrophy or retinal degeneration.
- Seizures
Hallervorden Spatz disease may possibly cause several other diseases including Cerebellar syndrome, Choreoathetosis, Chronic brain failure, Fits, Parkinsonism, Retinitis pigmentosa and Spastic ataxia.
Diagnosis of Hallervorden spatz disease
A neurological examination will reveal abnormal postures and movements, muscle rigidity, tremors and weakness. Genetic tests help to detect defective gene that causes the disease. However, this test is not widely available. MRI and similar other tests help to rule out the movement disorders and diseases.
Hallervorden Spatz disease gets worse and nerves are damaged over time. This leads to lack of movement and often death by early adulthood. Hence, treatment to control the symptoms becomes imperative. But there are no specific lines of treatment for HSD, consuming certain vitamins like panthothenate, Coenzyme Q10 and antioxidants can help the patient to some extent as they help ease the symptom severity. Sometimes medications used to treat symptoms for HSD can cause additional complications. These include blood clots, respiratory infections and skin breakdown.
Tags: #Deep Brain Stimulation #Niemann pick #Hallervorden spatz disease
At TargetWoman, every page you read is crafted by a team of highly qualified experts — not generated by artificial intelligence. We believe in thoughtful, human-written content backed by research, insight, and empathy. Our use of AI is limited to semantic understanding, helping us better connect ideas, organize knowledge, and enhance user experience — never to replace the human voice that defines our work. Our Natural Language Navigational engine knows that words form only the outer superficial layer. The real meaning of the words are deduced from the collection of words, their proximity to each other and the context.
Diseases, Symptoms, Tests and Treatment arranged in alphabetical order:

A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
Bibliography / Reference
Collection of Pages - Last revised Date: December 17, 2025



