Chemotherapy
Chemotherapy treatment works just after surgery; Being a systemic treatment, it attacks young and small clusters of cancer cells anywhere in the body. Chemotherapy drugs work best against rapidly dividing cells. The flip side is that they may kill normal cells too. Since cells in the blood, mouth, nose, nails and hair area also undergoing constant and quick division, chemotherapy affects them too. This explains the side effects of chemotherapy such as falling hair, dipping energy levels and infections. Supportive medicines are prescribed to help the body during this phase.
A typical treatment process may involve four to eight cycles of chemotherapy. Chemotherapy reduces the chances of cancer recurring after surgery. The tumors are shrunk with chemotherapy treatment, especially in cases of inflammatory cancer. The chemotherapy drugs are injected through IV needles. Sometimes they are given as pills. Oncologist will monitor your response to the therapy.
Side effects of chemotherapy
Breast Cancer
Breast cancer is the second deadliest cancer among women. But it has been noted that with increased awareness and thereby early detection and improved treatment, the number of deaths has reduced. But the incidence of breast cancer has been increasing steadily. Breast cancer is generally noticed in women above the age of 50 years. If a woman has sisters, mother or close blood relatives who have had breast cancer, she is more at risk. Women who have had an early menarche and late menopause are at higher risk for breast cancer. Lifestyle factors such as high alcohol consumption, obesity, diet rich in saturated fat and sedentary lifestyle increases a woman's risk for breast cancer. Long-term use of Hormone Replacement Therapy or HRT increases the risk of breast cancer.
Approximately 8% of breast cancers are hereditary and of these one-half are associated with mutations in genes BRCA1 and BRCA2. A history of a proliferative breast abnormality like atypical Hyperplasia may increase the risk for developing breast cancer. Women who have a family history of BRCA mutation should initiate annual mammography between 25 and 35 years of age. The selective estrogen receptor modulator tamoxifen or raloxifene lowers the risk of developing breast cancer.
Symptoms of breast cancer:
- Lump or thickening in or near the breast or in the underarm area.
- Prominently visible veins on the surface of the breast or peeling and scaling should not be ignored.
- Yellowish green discharge from the nipple can be a possible breast cancer symptom.
- Nipple discharge may be from infection which is usually purulent and from pregnancy, stimulation or prolactinoma which produces a thin, milky, often bilateral discharge. A suspicious discharge from a single duct can be evaluated
with a ductogram.
- Change in size, shape and appearance need to be carefully observed, as it can be a potential symptom of breast cancer.
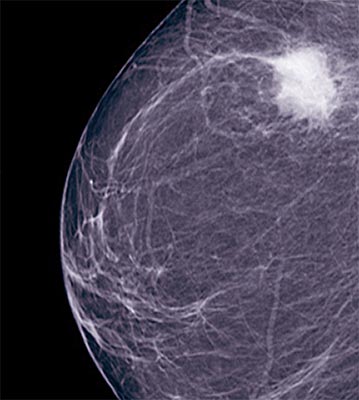
Every woman must learn to conduct a BSE (Breast Self Examination) to check for abnormal lumps, irregularities or discharge from the nipples. Such BSE combined with annual check ups by a doctor improves the chances of detecting breast cancer at an early stage. Palpate the breast tissue, axillary area and supra clavicular areas for masses or adenopathy. Physical examination of the breast should be performed in the upright and supine positions. Look for differences in size, retraction of the skin or nipple, prominent venous patterns and signs of inflammation. A mass that is suspicious for breast cancer is usually discrete, solitary, hard, unilateral and non tender. A Mammogram of the breast is routinely advised for women who are at higher risk for developing breast cancer. A clinically suspicious mass should be subjected to a biopsy even if mammography findings are normal.
Breast Cancer - Risk factors
- Family history of breast or ovarian cancer specifically with BRCA mutations
- History of breast cancer
- Increasing age
- Early age at menarche and late menopause.
- Prolonged exposure / higher concentrations of endogenous or exogenous estrogen
- Exposure to ionizing radiation
- Dense breast tissue
- atypical Hyperplasia
- Women with no children or who had their first child after the age 30
- Sedentary life style
- High fat content in diet
- Excessive Alcohol consumption
Though Bilateral mastalgia is rarely associated with breast cancer, it does not totally rule out the possibility. It is usually related to Fibrocystic changes in pre menopausal women with diffuse lumpy breasts.
Breast Cancer - Treatment Options
Appropriate breast cancer treatment is decided on the basis of a number of factors. Breast cancer treatment will depend on a number of factors such as size and location of the breast lump, the stage at which it was detected and the results of hormone receptor tests.
The most common approach for advanced breast cancer is preoperative chemotherapy followed by surgery and radiotherapy.
Surgery and chemotherapy are often used in combination. Chemotherapy is breast cancer treatment with anti-cancer drugs administered intravenously or orally. This systemic form of treatment is either administered alone or along with surgical procedures. Chemotherapy is a systemic therapy that affects the entire body by entering the bloodstream. This is used widely in breast cancer treatment to interfere with rapidly dividing cells. Radiation is the use of high-energy rays to prevent breast cancer cells from further growth and division. Though normal cells are also affected by this form of breast cancer treatment, they generally repair themselves and function normally afterwards. Adjuvant systemic therapy consists of administration of hormone
therapy, chemotherapy or trastuzumab (a monoclonal antibody directed against HER-2/neu). It benefits most women who are in the early stage of breast cancer, but the magnitude of benefit is greatest for those with node positive disease.
Myelodysplastic Syndrome
Myelodysplastic syndrome or MDS refers to a group of blood disorders caused by defective blood cell production in the bone marrow. Bone marrow produces immature blood cells called blasts, which over a period of time develop into mature blood cells and divide themselves into red blood cells, white blood cells and platelets. In Myelodysplastic syndrome, these blasts fail to mature and either die in the marrow itself or soon after they reach the blood stream. When there are not enough healthy blood cells, the body becomes weak and is susceptible to infections. MDS is not a cancer, however, in 20 to 30% of patients, the condition may progress itself into cancer and thus this condition was earlier called preleukemia.
Causes of Myelodysplastic syndrome
Based on causes, Myelodysplastic syndrome can be classified into primary MDS and secondary MDS. Myelodysplastic syndrome presenting itself without any known cause is called primary MDS. Myelodysplastic syndrome may also occur due to some known reasons such as history of cancer treatment involving radiation and chemotherapy, exposure to certain industrial chemicals and smoking. When the cause of the MDS condition is known, it is called secondary Myelodysplastic syndrome. Identifying the type of MDS is vital to the treatment as primary MDS has better prognosis when compared to secondary MDS.
Symptoms
Myelodysplastic syndrome does not cause any symptoms in the initial stages of the disease. However, the following warning signs may show up as the disease starts to progress.
- Fatigue due to anemia
- Frequent infections due to damaged immune system
- Shortness of breath
- Paleness
- Easy bruising or bleeding can occur due to low platelet count.
- Small red spots just under the skin.
Diagnosis and treatment
MDS is diagnosed with the help of blood tests and bone marrow tests. A complete blood test is done to understand the different blood counts. However, blood tests alone cannot detect MDS. Bone marrow tests are conducted to confirm the presence of Myelodysplastic syndrome. This procedure involves taking bone marrow samples from the pelvic bone of the patient by inserting a needle under local anesthesia. Once MDS is determined, the following methods are followed to treat the condition.
- Chemotherapy drugs
- Blood transfusion to treat anemia and low platelet count.
- Using medications called growth factors to allow the bones marrow to make more blood cells.
- Antibiotics to treat infections
- Stem cell transplant, an option that promises a cure to MDS, yet not widely adopted, as not many candidates qualify for this method. This method involves destroying the existing cells in the bone marrow via chemotherapy and radiation and infusing the stem cells from the donor.
At TargetWoman, every page you read is crafted by a team of highly qualified experts — not generated by artificial intelligence. We believe in thoughtful, human-written content backed by research, insight, and empathy. Our use of AI is limited to semantic understanding, helping us better connect ideas, organize knowledge, and enhance user experience — never to replace the human voice that defines our work. Our Natural Language Navigational engine knows that words form only the outer superficial layer. The real meaning of the words are deduced from the collection of words, their proximity to each other and the context.
Diseases, Symptoms, Tests and Treatment arranged in alphabetical order:

A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
Bibliography / Reference
Collection of Pages - Last revised Date: February 16, 2026



