Achromatopsia
Achromatopsia or Color Vision Deficiency - CVD is a relatively rare condition that manifests in many ways. The inability to differentiate red from green is probably the common form of color blindness that affects more men than women - 7 % of US male population as against just 0.4 % of female. But blue/yellow color vision problem, though rare, has no gender bias. Total color blindness or Achromatopsia is comparatively rare.
Color Perception: Every human retina has about 6 million cone cells of three types sensitive to the primary colors - Red, Green and Blue. The photo pigment each cone contains is specific to one particular light wavelength. A 'normal' color vision implies that all cone receptors have equal response to the narrow band spectrum of color human eyes can perceive.
Human retina also has 120 million Rod cells which can perceive fine details and gradations largely responsible for visual acuity. Thus it can be seen that a human eye is 'designed' to visualize more monochromatic details than details in color.
Causes of Achromatopsia: Most color deficiency issues are inherited. Other causes of acquired Achromatopsia can be due to the following chronic conditions:
- Diabetes Mellitus
- Glaucoma
- Macular Degeneration
- Retinitis Pigmentosa
- Multiple Sclerosis
- Alzheimer disease
- Parkinson disease
- Chronic Liver disease
- Sickle cell anemia
Some drugs such as antibiotics, antihypertensive, barbiturates and drugs to treat psychological and CNS conditions can affect the color vision. Industrial chemicals like CO, fertilizers, solvents and lead can hurt the color vision on prolonged exposure.
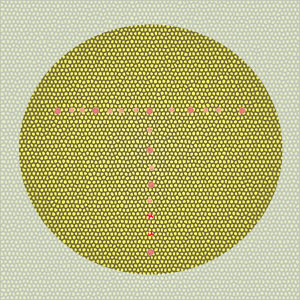
Diagnosis: There are many visual tests available to diagnose color perception deficiency - American Optical Pseudoisochromatic test plates, Titmus vision tester and Ishihara test to name a few. These tests contain color coded patterns or numbers against another set of colored background.
Treatment: There is no treatment for inherited color blindness. In the case of acquired color deficiency problems, removal of the causative condition may help to regain normal color perception over a period of time. But usually there is poor prognosis for most color blindness conditions. Most patients generally adapt to their abnormality by looking for other subtle cues.
Optic Neuritis
Sudden inflammation of the optic nerve resulting in reduced vision in the affected eye is 'optic neuritis'. In particular, the myelin lining of the optic nerve which transmits visual stimuli to the brain is inflamed. As it is the optic nerve that carries visual information from the retina to the brain stem, vision is affected when the optic nerve is impaired. Optic Neuritis is also called Retro-bulbar neuritis.
Although the precise cause of Optic Neuritis is unknown, it is an autoimmune disorder. It usually occurs in children and young adults below 40 years of age. It can involve one or both optic nerves. It is more common in females. The annual incidence is approximately 6.4 / 100,000. Studies also reveal that about 1 in 5 patients who have had a first episode of optic neuritis are likely to develop nerve problems elsewhere in the body, or will develop multiple sclerosis.
Normally, the body's immune system fights infection by creating a reaction that can combat viruses, bacteria, fungi and others. But in autoimmune diseases, this reaction is directed against a normal part of the body instead of the inflamed part. In case of Optic Neurosis, there occurs inflammation and destruction of the protective myelin sheath that insulates the optic nerve by coating it and direct damage to the nerve axons leads to loss of vision.
In Optic Neurosis, the loss of vision can be sudden or develop gradually over a period of time. Vision loss may be partial or complete or may be only a certain part of the visual field. It is recommended that a person experiencing a first episode of Optic Neuritis undergo MRI of the brain. This can help identify for central nervous system lesions and the MRI can reveal an enlarged optic nerve. Other symptoms include loss of vision in one eye even for an hour, loss of color vision (achromatopsia), changes in pupil's reaction to bright light, and pain when the eye is moved.
Appropriate therapy is instituted depending upon the underlying cause of the infection in case of other autoimmune diseases. In some cases there can be no conclusive treatment as even oral and intravenous steroids, when used in treatment, do not have any long-term acuity and instead risks of side effects can be significant in some patients.
However, there are chances that normal vision returns within 2 to 3 weeks with no treatment. Corticosteroids given intravenously may speed up recovery whereas oral steroids may increase the chance of recurrence. Further evaluation can determine the cause of Neuritis and the underlying condition causing the problem can be treated.
Tags: #Achromatopsia #Optic Neuritis
At TargetWoman, every page you read is crafted by a team of highly qualified experts — not generated by artificial intelligence. We believe in thoughtful, human-written content backed by research, insight, and empathy. Our use of AI is limited to semantic understanding, helping us better connect ideas, organize knowledge, and enhance user experience — never to replace the human voice that defines our work. Our Natural Language Navigational engine knows that words form only the outer superficial layer. The real meaning of the words are deduced from the collection of words, their proximity to each other and the context.
Diseases, Symptoms, Tests and Treatment arranged in alphabetical order:

A B C D E F G H I J K L M N O P Q R S T U V W X Y Z
Bibliography / Reference
Collection of Pages - Last revised Date: February 23, 2026



